Creating the Body Electric
Premature babies are fragile, and their health status needs to be monitored 24-7, so that if any problem occurs, healthcare providers can engage immediately. In the neonatal intensive care unit (NICU), this is normally accomplished with monitoring systems made up of hard-wired, rigid interfaces attached with tape to a neonate's fragile, underdeveloped skin. In some cases, invasive lines are inserted into their delicate arteries. These interfaces pose risks for skin injuries, either from removing the tape or simply from the infant's natural movements. They also create physical barriers to parent/child interactions and basic clinical tasks.
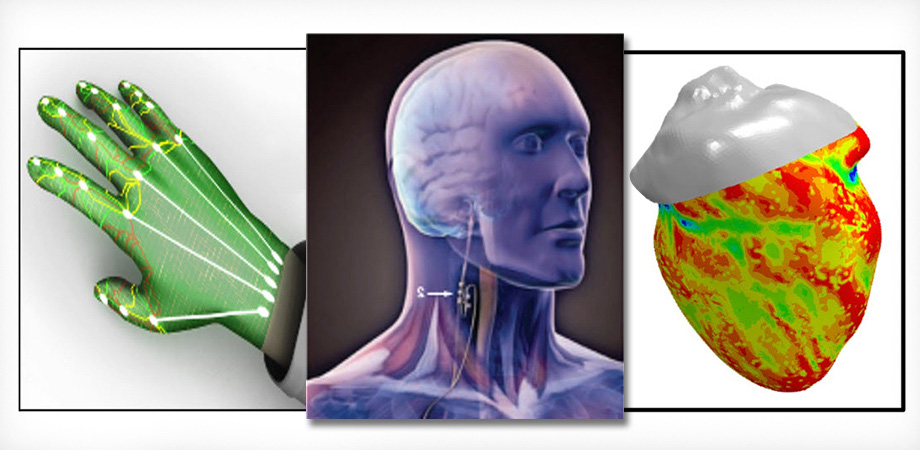
As an answer to this problem and similar issues, SPIE Fellow John A. Rogers and his team at Northwestern University have developed innovative NICU monitoring technology that can interface with the soft, curvilinear textures of the body, such as the brain, the heart, and the skin. Rogers' team recently completed a four-year project, producing these monitoring devices that, when used in a time-synchronized fashion, can reconstruct complete vital sign information with clinical-grade precision.
"These wireless, skin-like devices can really do everything we were hoping they could do," Rogers told an audience at SPIE Defense + Commercial Sensing in April. "We can get rid of this rat's nest of wires and replace that type of technology with something more humane and much more friendly to the baby."

Soft, biocompatible sensors will make time in NICU less stressful. Credit: John Rogers/Northwestern University
Rogers, the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery at Northwestern, added that the project is scheduled to deploy 20,000 of the skin-and baby-friendly units to India, Pakistan, and Zambia over the coming year, with funding from the Bill & Melinda Gates and Save the Children foundations.
A future phase of implementation is to get these devices into the home. "The parents we talk to are very stressed out when their babies are in the NICU," said Rogers. "it's even worse when they have to take them home, because then they're flying blind, they don't know what's going on. So, being able to take the baby home with monitoring hardware at the same time and being able to send that data to the neonatologist I think will be a very natural next step."
Expanding the interface
Rogers' keynote address, "Some Recent Progress in Skin-Interfaced Electronics" included descriptions of work on other sensors that aid patients such as those with hydrocephalus, a condition where excess cerebrospinal fluid builds up in the ventricles of the brain. The current standard of care is to insert a shunt to drain that fluid away from the brain. Shunts often clog, causing nonspecific symptoms such as headaches, dizziness, and nausea, and there is no non-invasive way to check the shunt to ascertain if it's working properly. As an example, Roger's showed a short film about a 36-year-old man who, since childhood, had undergone 189 surgical procedures related to his shunt. The film showed how Rogers' device, a wireless, flexible sensor, can successfully test these shunts; within five minutes of being placed on the skin, the sensor can measure whether fluid is flowing through the shunt, by use of a thermal actuator. "It's based on a thermal transport measurement," said Rogers. "We dose in very tiny amounts of thermal power, increase the temperature locally in the skin by a very slight amount, and then measure the change in temperature that's induced by flow or no flow through the shunt. From the patient's perspective, it looks like a Band-Aid that's talking to your cell phone."
The research team at Northwestern is collaborating with other groups on several projects. Credit: John Rogers/Northwestern University
Rogers' team is developing other sensors for rehabilitation and healthcare that are currently being tested in hospital settings. Examples include sensors that check for peripheral nerve monitoring in the operating room; tremor/EMG monitoring in Parkinson's patients; motion/EMG monitoring in stroke rehabilitation; and cardiac/stress monitoring in expecting mothers.
"What we focus on are mesh-type constructs," said Rogers, "These are filamentary serpentine structures that form an interconnected mesh which when integrated with the soft, elastomeric substrate, can yield effective, stress/strain properties that can be matched to targeted biological systems of interest, even in platforms that incorporate high-modulus, inorganic semiconductors on those filaments. They are almost imperceptible to the wearer. We can embed all sorts of advanced sensor functionality, microprocessor computing capability, power supplies, etc., into this platform, and that is the uniqueness of what we do."
The uniqueness of these designs, demonstrating, in part, the merging of art and science, earned Rogers' work a spot in a 2017 Museum of Modern Art (MoMA) exhibit that showed how fashion and functionality can be combined through design and technology. The item on display was a "bio-integrated lab" - a soft, flexible microfluidic system that takes minute samples of sweat and performs chemical analysis of key biomarkers such as pH, lactate, chloride, and glucose.
The bio-integrated lab design earned a spot in a 2017 exhibit at the Museum of Modern Art. Credit: John Rogers/Northwestern University
In an interview with MoMA, Rogers noted that his team was "pretty good at science and engineering," but he never thought their work would be considered artistic. He added, however, that people might be hesitant to wear something on their skin that looks like a medical device. "The devices we're building meet these unique physical, engineering challenges in intimate, comfortable, and non-irritating integration with the body, but the emotional judgments are just as important," said Rogers. "As engineers, we have to consider these things."
Collaboration is key
In a Q&A session after the talk, Rogers was asked what advice he had for students and up-and-coming researchers who are translating their technologies into applications.
"I think a lot of this kind of translational work requires so many different experts in different disciplines that you really have to learn to work effectively with other groups - multiple other groups in many cases," said Rogers. He referenced a recent paper published in Science - "Binodal, wireless epidermal electronic systems with in-sensor analytics for neonatal intensive care" - in which Rogers and 44 co-authors wrote about the sensors being developed for premature babies in NICUs. These authors spanned nearly every field of engineering science and relevant areas of clinical medicine.
"Teaching your students how to do that is going to be very powerful for them as they move through their career," Rogers continued. "Being able to engage with people in adjacent disciplines and being able to work effectively with them as part of a broader team, while also leveraging your own expertise and driving your own projects; not sacrificing those projects, but enabling yourself to go further than you otherwise would be absent those kinds of collaborations."
| Enjoy this article? Get similar news in your inbox |
|



